Le TAVI Pour la vie (Redo TAVI)
TAVI
Julien Adjedj MD, PhD
4/9/20245 min read
Le TAVI pour la Vie!
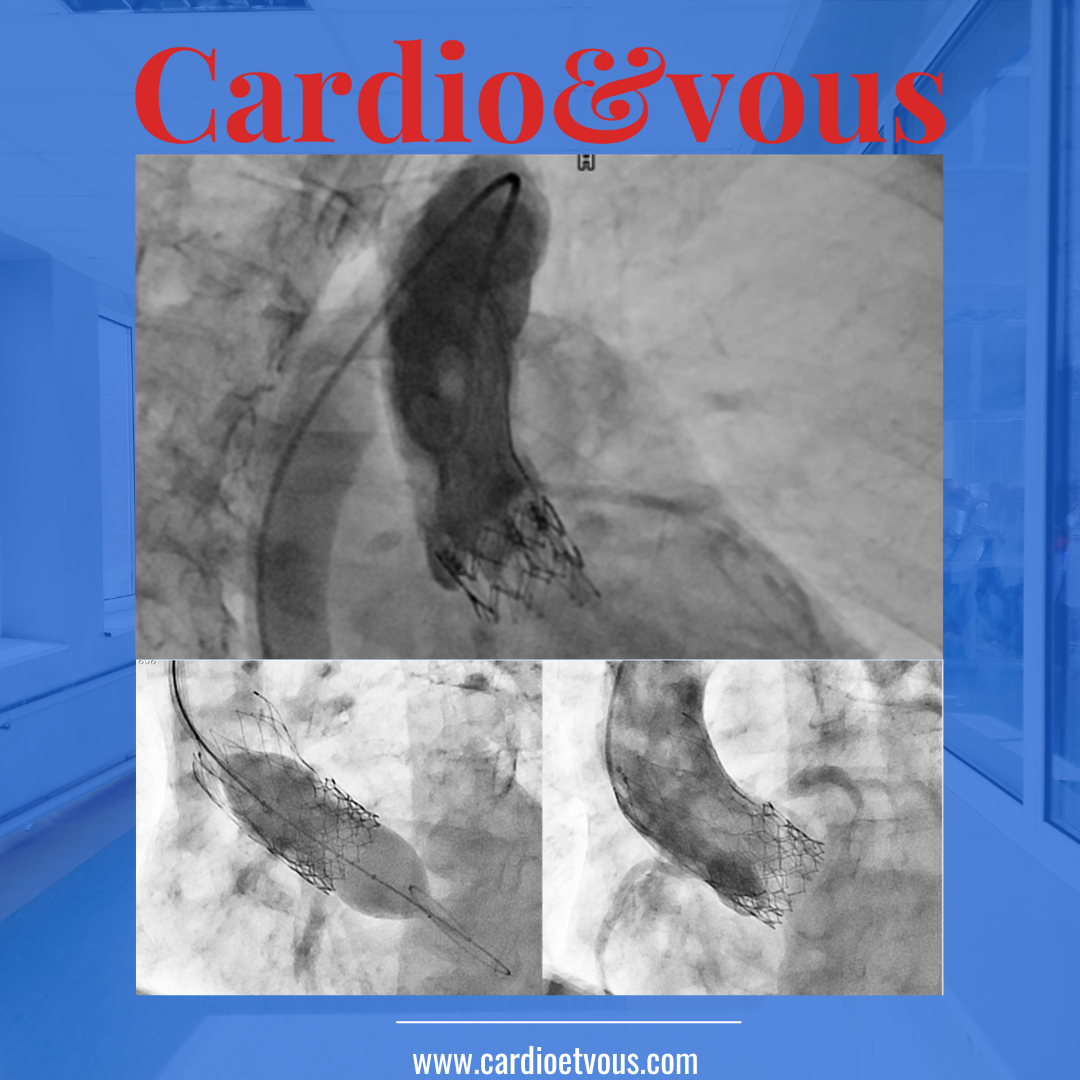
Redo Transcatheter Aortic Valve Implantation (TAVI), a minimally invasive alternative to traditional open-heart surgery, offers hope for patients at high risk for surgical complications. This procedure, which involves guiding a new valve to the heart through a catheter, has become a cornerstone in the treatment of severe aortic stenosis, significantly enhancing patients' quality of life and heart function.
With the first TAVI procedure marking its inception in 2002, the method has since transformed into a critical aspect of cardiac medicine, serving over 300,000 patients worldwide. Its success underlines the procedure's high efficacy rate and the pivotal role it plays in contemporary cardiologie interventionnelle.
The Evolution and Necessity of Redo TAVI
The evolution of Redo TAVI has been marked by significant advancements and the necessity of addressing complex challenges associated with repeat procedures. Key developments include:
Utilization of computer modeling to predict outcomes, reducing risks in redo TAVI surgeries.
The Valve Academic Research Consortium's updates on clinical endpoints for TAVI, including Bioprosthetic Valve Dysfunction (BVD) and Structural Valve Deterioration (SVD).
Outcomes and Preferences:
Meta-analysis showing lower 30-day mortality rates for valve in valve (ViV) TAVR compared to redo-SAVR.
High device success rate (85.1%) and acceptable peri-procedural complication rates in redo-TAVI.
Preference for redo TAVI in younger, less comorbid aortic stenosis patients due to increased life expectancy.
Anatomical Considerations and Future Directions:
Lack of data on preserving coronary arteries and future coronary access in redo-TAVI.
CT-based simulations by Grubb et al. to evaluate anatomical feasibility of redo-TAVI, highlighting the importance of Evolut stent frame positioning for optimal coronary flow and access.
Factors increasing the risk of coronary flow compromise, emphasizing the need for careful anatomical assessment.
The growing necessity of redo-TAVI for patients with longer life expectancies outliving their transcatheter heart valves, underscoring the importance of established treatment strategies for re-intervention.
Choosing the Right Valve for Redo TAVI
In the realm of Redo TAVI, selecting the appropriate valve is crucial for optimizing patient outcomes and minimizing procedural risks. This selection is guided by a comprehensive understanding of valve types, anatomical considerations, and patient-specific factors:
Valve Types and Considerations:
CoreValve/Evolut and Sapien: These valves are the most studied for valve-in-valve TAVI, with the Sapien valve displaying a higher incidence of postprocedural gradients in small surgical bioprostheses.
Navitor: Known for its fully retrievable feature, it offers an advantage in cases of potential coronary obstruction, despite the lack of substantial data supporting this. It also offers good hemodynamic performance for annular valve.
JenaValve and Centera/Acurate neo: The JenaValve is beneficial for pure aortic regurgitation due to its clipping mechanism, while Centera and Acurate neo valves are preferable in patients with coronary artery disease due to their lower frame height and short stent component.
Anatomical and Patient-Specific Factors:
The risk of coronary obstruction is more dependent on the geometry of the valve and sinuses rather than the TAVI valve type. Heavy calcification of the left ventricular outflow tract and annulus increases the risk of PVL and annular rupture, necessitating careful valve selection.
Bicuspid aortic valves, characterized by larger annulus dimensions and heavy calcification, may benefit from valves that offer minimal PVL, retrievability, and the option for repositioning.
Long-Term Durability and Redo Considerations:
CoreValve/Evolut and Sapien platforms have amassed significant data supporting their long-term durability. However, in instances of significant structural valve deterioration, a redo TAVI-in-TAVI procedure might be necessitated, heavily influenced by the patient’s anatomy.
Through meticulous preprocedural planning and consideration of these factors, clinicians can enhance the success rates of Redo TAVI procedures, providing patients with improved outcomes and quality of life.
Anatomical Considerations and Preprocedural Planning
Anatomical Considerations and Preprocedural Planning are pivotal in ensuring the success of a redo-TAVI procedure. This phase involves a meticulous assessment of various factors:
Prosthesis Information from Initial Procedure:
Valve type and size, neoskirt height, sinotubular junction (STJ) diameter, and coronary height are critical data points collected to tailor the redo-TAVI approach effectively.
Vessel and Valve Dimensions:
The minimal vessel dimensions required for successful transfemoral (TF) access are determined by the delivery system and the size of the transcatheter heart valve (THV).
Preprocedural computed tomography (CT) imaging with three-dimensional reconstruction is indispensable for accurately measuring the luminal diameter.
Anatomical Challenges:
Horizontal aorta and excessive aortic angulation may complicate the procedure, particularly with self-expanding THVs.
Presence of a concomitant aortic aneurysm requires a nuanced approach, factoring in the patient's surgical risk and life expectancy.
Bicuspid aortic valve (BAV) morphology, large annular dimensions, and calcified raphe increase the risk of paravalvular leak (PVL), new pacemaker implantation, and annular rupture.
Preprocedural planning also entails the use of ultrasound guidance to pinpoint the optimal femoral artery puncture site, minimizing vascular complications. The EuroSCORE and STS Short-Term Risk Calculator are employed to evaluate the patient's mortality and morbidity risk, assisting in the decision-making process between SAVR and TAVI. This comprehensive assessment ensures a tailored and safe approach to redo-TAVI, addressing both anatomical and procedural complexities. New application Redo TAV could help as well.
Future Directions and Technological Innovations
The landscape of transcatheter aortic valve implantation (TAVI) is rapidly evolving with the introduction of innovative technologies and valve designs aimed at enhancing procedural success and long-term outcomes. Noteworthy advancements include:
SAPIEN X4 with Resilia Valve (Edwards Lifesciences): Features anticalcification technology, a novel frame design, and a delivery system with THV rotation control.
Evolut FX SE (Medtronic): Offers a symmetric and predictable implant depth, with capabilities for recapturing and repositioning, suited for a wide range of vascular anatomies.
Navitor (Abbott Structural Heart): A self-expanding, resheathable, and partially retrievable THV with enhanced visibility and three bovine pericardial tissue valve leaflets.
Acurate neo2 (Boston Scientific): Known for its self-expanding mechanism, porcine pericardial tissue, and a design that ensures axial alignment.
JenaValve Trilogy: Specifically targets pure aortic regurgitation (AR), offering three sizes for optimal fit and delivered via an 18F Coronatix catheter.
RESILIA Tissue (Edwards Lifesciences): A bovine pericardial tissue with anticalcification technology, aiming to extend valve durability.
DurAVR THV System (Anteris Technologies): Features a unique leaflet design that mimics native valve anatomy, potentially improving long-term performance.
Foldax Tria Heart Valve: Utilizes a novel polymer-based leaflet material (TRIA LifePolymer) designed for durability and longevity.
These technological innovations represent a significant leap forward in TAVI, focusing on improving patient outcomes, procedural safety, and the long-term durability of bioprosthetic valves. As these new devices undergo clinical evaluation and gain wider adoption, they promise to further refine the TAVI landscape, offering more personalized and effective treatment options for patients with aortic valve diseases.
FAQs
What is the expected lifespan following a TAVI procedure?
Following a TAVI (Transcatheter Aortic Valve Implantation) procedure, studies have indicated that the life expectancy rates are 92.9% at 30 days post-procedure, 78.6% at one year, and 73.7% at two years. It has also been observed that the transfemoral approach to TAVI may offer better survival outcomes compared to other vascular access methods.
Is it possible to replace a TAVI valve more than once?
Yes, it is possible to replace a TAVR valve more than once. If a patient requires a second valve replacement, another tissue valve can be placed inside the previously implanted valve through another TAVR procedure. However, if a surgical approach is necessary, the existing valve(s) must be surgically removed before a new one can be implanted.
Can a TAVI procedure be redone?
Recent studies have confirmed that redoing a TAVR procedure is both a safe and effective option. These findings apply even when comparing redo TAVR procedures to initial TAVR procedures in patients with similar risk profiles, highlighting the procedure's reliability and effectiveness even when performed a second time.
References
[1] - https://www.mayoclinic.org/tests-procedures/transcatheter-aortic-valve-replacement/about/pac-20384698
[2] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10875938/
[3] - https://www.jacc.org/doi/10.1016/j.jcin.2023.07.034
[4] - https://www.mdpi.com/2077-0383/12/14/4788
[5] - https://eurointervention.pcronline.com/article/being-prepared-for-redo-tavi-in-self-expanding-evolut-valves-important-insights
[6] - https://eurointervention.pcronline.com/article/aortic-stenosis-management-current-evolution-and-future-challenges
[7] - https://www.ajconline.org/article/S0002-9149(23)00010-3/fulltext
[8] - https://citoday.com/articles/2019-mar-apr/tavi-which-valve-for-which-patient
[9] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8076502/
[10] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9390471/
[11] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10198244/
